March 28, 2021
Effect of race and ethnicity on influenza vaccine uptake among older US Medicare beneficiaries: a record-linkage cohort study. The Lancet Healthy Longevity
Summary
Background
Seasonal influenza vaccine (SIV) uptake among US adults aged 65 years or older remains suboptimal and stagnant. Further, there is growing concern around racial and ethnic disparities in uptake. We aimed to assess racial and ethnic disparities in overall SIV and in high-dose vaccine (HDV) uptake among Medicare beneficiaries during the 2015–16 influenza season and sought to identify possible mediators for observed disparities.
Methods
We did a historical record-linkage cohort study using Medicare (a US national health insurance programme) databases, which included all older adults (≥65 years) enrolled in Medicare during the study period (July 1, 2015, to June 30, 2016). We excluded beneficiaries of Medicare Part C (managed care offered by private companies), and residents of long-term care facilities. The primary outcome was SIV receipt during the study period, classified into receipt of HDV and standard-dose vaccines (SDVs, representing all other SIVs). SIV uptake probabilities were estimated using competing-risk survival analysis methods. Mediation analyses were done to investigate potential mediators of the association between race and ethnicity and uptake.
Findings
During the study period, of 26·5 million beneficiaries in the study cohort, 47·4% received a SIV, 52·7% of whom received HDV. Compared with white beneficiaries (49·4%), Hispanic (29·1%), Black (32·6%), and Asian (47·6%) beneficiaries were less likely to be vaccinated and, when vaccinated, were less likely to receive HDV (37·8% for Hispanic people, 41·1% for Black people, and 40·3% for Asian people, compared with 53·8% of white people who received HDV). Among those vaccinated, after accounting for region, income, chronic conditions, and health-care use, minority groups were 26–32% less likely to receive HDV, relative to white people (odds ratio [OR] 0·68 [95% CI 0·68–0·69] for Black people; OR 0·71 [0·71–0·72] for Asian people; and OR 0·74 [0·73–0·74] for Hispanic people).
Interpretation
Substantial racial and ethnic disparities in SIV uptake among Medicare beneficiaries aged 65 years or older are evident. New legislative, fiscal, and educational strategies are urgently needed to address these inequities.
Funding
Sanofi Pasteur.
Introduction
In the USA, annual administration of a seasonal influenza vaccine (SIV) is recommended for people at high risk of serious illness and death due to influenza, including all adults aged 65 years or older, who account for most influenza-related deaths and hospital admissions.1 However, SIV uptake among this age group remains suboptimal, levelling off at approximately 65% since 1998.2, 3 Concern is also growing about racial and ethnic disparities in SIV uptake. In a meta-analysis in 2019, we found that community-dwelling (non-institutionalised) Black and Hispanic adults aged 65 years or older had consistently lower SIV uptake than white adults, with pooled relative risk estimates of 0·60 (95% CI 0·49–0·73) for Black adults and 0·69 (95% CI 0·53–0·89) for Hispanic adults.4 However, the reviewed studies had substantial limitations, including reliance upon self-reported vaccination history, thus increasing the chance of recall and social desirability bias.4 Furthermore, it is unclear whether these disparities in uptake are the result of racial and ethnic differences in attitudes towards vaccination, which are known to be important determinants of SIV uptake, or the result of structural and systemic differences in access to high-quality vaccination services.4
The high-dose vaccine (HDV; Fluzone high-dose, Sanofi Pasteur, Swiftwater, PA, USA), a trivalent, inactivated, unadjuvanted SIV containing 60 μg of haemagglutinin per vaccine virus strain, was licensed in 2009 for adults aged 65 years or older as an alternative to the standard-dose vaccine (SDV), which contains only 15 μg of haemagglutinin per strain.5 In both immunogenicity and clinical efficacy trials, HDV was superior to trivalent SDV in this age group, probably because of its ability to elicit a stronger immune response in immunosenescent individuals.5 HDV, although widely used in the USA,6 is not preferentially recommended for adults aged 65 years or older, with the choice between HDV or SDV administration left to the individual and their health-care provider. This scenario provided a unique opportunity to explore racial and ethnic disparities in the receipt of a novel, more effective product (ie, HDV), compared with SDV, as both products have the same indication as well as financial incentives, as there are no out-of-pocket expenses for receipt of either vaccine.
Research in context
Evidence before this study
Seasonal influenza vaccine (SIV) uptake among adults aged 65 years or older in the USA remains suboptimal, and there is growing concern about racial and ethnic disparities in uptake. In a 2019 meta-analysis, we found that community-dwelling (non-institutionalised) Black and Hispanic adults aged 65 years or older are consistently less likely to receive a SIV than white adults of the same age range. We searched MEDLINE, Embase, CINAHL, and Scopus bibliographic databases for population-based clinical trials or observational studies that investigated determinants of influenza vaccine uptake, published between Jan 1, 2000, and Dec 31, 2017, in English (search terms used are provided in the appendix pp 4–5), and included those studies that were done in community-based older individuals (≥65 years) in the USA or Canada, irrespective of health status. However, the reviewed studies had substantial limitations, including reliance upon self-reported vaccination history, thus increasing the chance of recall and social desirability bias. Furthermore, it is unclear whether disparities in uptake are the result of racial and ethnic differences in attitudes towards vaccination or the result of structural and systemic differences in access to high-quality vaccination services.
Added value of this study
The availability of high-dose vaccines (HDVs) alongside standard-dose influenza vaccines in the USA, two types of influenza vaccines with the same indication and financial incentives, created a unique opportunity to explore disparities in SIV uptake. In addition to identifying substantial inequities in overall SIV uptake by race and ethnicity among US Medicare beneficiaries aged 65 years or older, we further showed that these inequities persist even among those who received, and presumably wanted, influenza vaccination, with minority groups having been significantly less likely to receive a novel, more effective product (ie, HDV). By limiting part of the analysis to people who were vaccinated, we effectively ruled out several often-cited justifications for inequities in vaccine uptake, such as higher amounts of vaccine hesitancy and distrust of public institutions among minority groups, living circumstances (eg, homelessness), or limited physical access to preventive services.
Implications of all the available evidence
In our study, substantial racial and ethnic disparities in SIV uptake among Medicare beneficiaries aged 65 years and older in the USA were evident, and these disparities even persisted among those who were vaccinated. New legislative, fiscal, and educational strategies are urgently needed to address these inequities.
We aimed to use de-identified Medicare data to assess racial and ethnic disparities in the receipt of HDV among community-dwelling Medicare beneficiaries aged 65 years or older who received a SIV during the 2015–16 influenza season. We also used mediation analysis to identify possible mediators for any observed disparities and assessed racial and ethnic disparities in the receipt of any SIV.
Methods
Study design and participants
We did a historical record-linkage cohort study. The sociodemographic and medical determinants of SIV and HDV uptake in this cohort have been previously detailed.7 In this Article, we focus on analysing racial and ethnic disparities with two approaches: a time-to-event (survival) analysis of all beneficiaries to assess racial and ethnic disparities in the receipt of any SIV; and a logistic regression analysis, limited to beneficiaries who received a SIV, to measure racial and ethnic disparities in the receipt of HDV.
We included all beneficiaries in Medicare during the study period of July 1, 2015, to June 30, 2016, thereby spanning the 2015–16 influenza season, who were aged 65 years and older at the study start date. We excluded beneficiaries of Medicare Part C, known as Medicare Advantage (managed care offered by private companies), because their information is not captured in Centers for Medicare and Medicaid Services’ (CMS) databases, and residents of long-term care facilities, because both their probability of vaccination and their vaccine choices are probably determined by facility policies. The study population formed a dynamic cohort; participants entered the cohort on either the study start date (July 1, 2015), the date coverage was initiated, or their 65th birthday. They exited the cohort on either the date of death, date of termination of coverage, study end date (June 30, 2016), date of admission to a long-term care facility, or date of SIV administration. To ensure a sufficient follow-up time, we excluded participants who had less than 3 months of coverage.
The study was approved by the CMS privacy board. As a retrospective study, there was no formal involvement of patients and the public in this study; therefore written informed consent was not required.
Procedures
Medicare is a US Federal health insurance programme that provides free or subsidised coverage for inpatient hospital and hospice care (Part A) to more than 55 million beneficiaries, including 98% of US adults aged 65 years or older, as well as younger people with disabilities and patients with end-stage renal disease.8, 9, 10 More than 96% of beneficiaries are also enrolled in Medicare Part B, which covers medically necessary clinician services and other outpatient services, whereas about 70% are also enrolled in Part D, which provides prescription drug coverage.10 Both Part B and D charge premiums and all parts entail additional out-of-pocket expenses owing to required co-payments and deductibles.
Person-level data on health service use for all Medicare beneficiaries was obtained from the CMS.11 The CMS’s Master Beneficiary Summary File contains demographic information (including race and place of residence) and enrolment status in each Medicare programme part, and flags existing chronic conditions (defined using the CMS’s Chronic Condition Data Warehouse case definitions).12 It also contains an encrypted beneficiary identification number that can be used to link to the Medicare carrier files and Medicare outpatient files, which provide information on all claims submitted for physician and nursing services provided in ambulatory and hospital outpatient settings. These files include information on the nature and date of provided services, coded using the Current Procedural Terminology, and on diagnoses, coded using the tenth edition of the International Classification of Diseases.11 Hospital admission information was obtained from the cost and utilisation segment of the Master Beneficiary Summary File.
Outcomes
The primary outcome was the first receipt of a SIV during the study period. Subsequent records of SIV vaccination were excluded (n=46 233; about 0·2% of all vaccination records captured). SIV administration was identified using Current Procedural Terminology codes as recorded in the CMS carrier and outpatient files. We classified SIVs into HDV (Fluzone high-dose) and SDV (all other SIVs).
Race is a social, rather than biological, construct, deeply rooted in historical and contemporary economic and political power differentials within society. The CMS routinely gathers beneficiary race and ethnicity information in accordance with an Office of Management and Budget directive.13 Neither concept was defined explicitly by this directive, but the term race refers to self-reported (when applying for a social security number) geographical origin, whereas ethnicity refers to whether someone is Hispanic. There were five racial categories in the CMS: white (having origins in Europe, the Middle East, or North Africa); Black (having origins in any of the Black racial groups of Africa); American Indian or Alaska Native (having origins in the original peoples of North and South America, and maintaining tribal affiliation or community attachment); Asian (having origins in the Far East, southeast Asia, or the Indian subcontinent); and Native Hawaiian or Other Pacific Islander (having origins in Hawaii or other Pacific Islands).13 In all analyses, we used the combined race and ethnicity groupings provided by the CMS (table 1), except for grouping Native Hawaiian and Other Pacific Islanders with people of mixed race as Other, because of their small numbers.
To explore regional differences, we assigned participants to one of five US census bureau regions: northeast, midwest, south, west, and US territories, and to either an urban or rural area using the CMS’s rural area definition (postcode [zip code] that is mostly non-metropolitan).14 We used two approaches to measure the intensity of health-care service use: (1) the number of inpatient admissions, outpatient emergency room visits, physician visits, and Part D prescriptions in 2015; and (2) overall use cost categorised based on the percentiles of the total annual Medicare expenditures in 2015 into five groups: crisis (99th percentile), heavy (90th to 98th percentiles), moderate (75th to 89th percentiles), light (50th to 74th percentiles), and low consumption (1st to 49th percentiles).
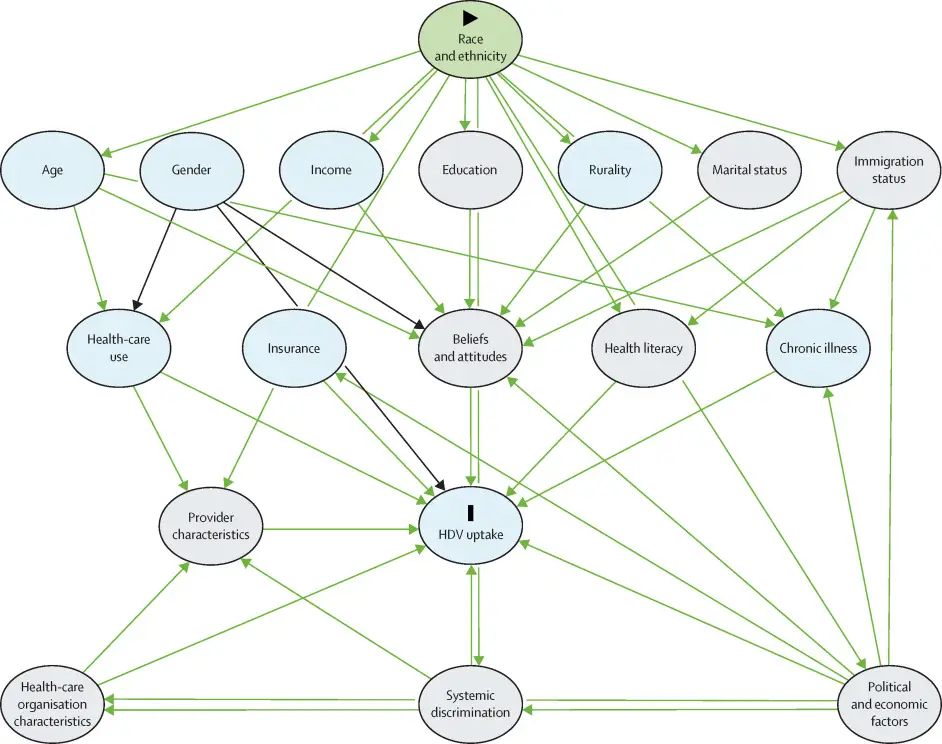
Statistical analysis
We estimated the probability of receiving any SIV during the 2015–16 season using competing-risk survival analysis methods, with death and transfer to a long-term care facility as competing risks. Unlike standard survival analysis methods, this approach does not assume that these competing events are independent.16 We used Cox models to estimate hazard ratios (HRs) and 95% CIs for the association between race and ethnicity and SIV.16 We did mediation analyses using the Baron–Kenny framework (figure),17 according to a prespecified causal diagram (a directed acyclic graph).18 In our directed acyclic graph, which was developed during a consultation session with experts and stakeholders (Nov 19, 2017), we treated race as an antecedent cause (ie, preceding cause) of most other vaccine uptake determinants, such as age, region of residence, income (measured using Part D low-income subsidy as a proxy), chronic diseases, and patterns of health-care use (ie, we consider these factors mediators rather than confounders of race’s effect on vaccine uptake). Using the Baron–Kenny decomposition, we verified that race and ethnicity was correlated with SIV uptake and with the mediator variables, which are also correlated with SIV uptake.
In analyses restricted to recipients of a SIV, we used logistic regression models to estimate odds ratios (ORs) and 95% CIs for the association between race and receipt of HDV (vs SDV). To assess effect modification, we tested for multiplicative interactions between race and several vaccination determinants, including age, gender, region of residence, income, chronic conditions, and patterns of health-care use using likelihood ratio tests.19 All analyses were done using SAS, version 9.4.
Role of the funding source
The funder of the study reviewed both the study protocol and final manuscript, but had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Between July 1, 2015, and June 30, 2016, we included 26·5 million beneficiaries who met all inclusion criteria in our cohort. White people, representing 86·1% of the cohort, were more likely to be aged 75 years or older, compared with Black and Hispanic people (table 1). Women comprised a higher proportion of the Black (59·1%) and Asian beneficiaries (59·9%) than the white (56·1%) and Hispanic beneficiaries (56·9%). A larger proportion of white people (23·4%) resided in rural areas relative to all other racial and ethnic minority groups. Fewer Hispanic people had a documented chronic disease (64·6%) than other groups (range 67·2–70·7%). A higher proportion of Asian people had no hospital admissions during the study period (90·1%) compared with other groups (range 84·3–88·7%). Fewer Asian people also visited an emergency room (10·5% had one visit, 4·1% had ≥2), but a higher proportion had at least one Part D prescription filled (70·5% had ≥1 or more filled).
Across the cohort, 47·4% of participants received a SIV and, of those, 52·7% received the HDV (table 2). Women were more likely to have been vaccinated (49·5% vs 44·8% for men) but were slightly less likely to have received the HDV (52·1% vs 53·6% for men). Compared with white people (49·4%), Hispanic (29·1%), Black (32·6%), and Asian (47·6%) people were less likely to have been vaccinated, and for those who were vaccinated, less likely to have received the HDV (37·8% for Hispanic people, 41·1% for Black people, and 40·3% for Asian people compared with 53·8% for white people). Similarly, rural residents were less likely to have received a SIV (21·7%) and, for those who were vaccinated, less likely to have received the HDV (45·3%), compared with urban residents. People with chronic diseases were more likely to have been vaccinated (54·0% vs 32·9% for those without a chronic diagnosis), but less likely to have received the HDV (51·1% vs 58·7% for those without a chronic diagnosis). More frequent physician visits were associated with a greater likelihood of receiving a SIV, but not with receiving the HDV. A crisis level or heavy level of health-care use was associated with a lower likelihood of receiving a SIV and the HDV. Low-level health-care use was also associated with a low SIV uptake (40·5%).
Racial and ethnic disparities in SIV uptake persisted even after accounting for differences in age and gender (table 3); Hispanic people (48%; HR 0·52 [95% CI 0·51–0·52]) and Black people (41%; HR 0·59 [0·58–0·59]) were less likely to have been vaccinated than white people. In the mediation analysis, the gap narrowed to 30% (adjusted HR 0·70 [95% CI 0·70–0·71]) for Hispanic people and 34% (adjusted HR 0·66 [0·66–0·66]) for Black people after additionally accounting for region of residence, income, chronic conditions, and patterns of health-care use (full model), suggesting that these factors might partly mediate, but not fully, the effect of race on SIV uptake.
In the full model, the strongest predictors of SIV uptake were having more than ten physician visits (HR 2·55 [95% CI 2·54–2·55]), followed by filling more than 30 prescriptions (HR 1·55 [1·55–1·56]), and having a chronic condition (HR 1·29 [1·28–1·29]). By contrast, more frequent hospital admissions and emergency room visits were associated with lower vaccine uptake, as were receiving a low-income subsidy (HR 0·71 [95% CI 0·71–0·71]) and residing in rural areas (HR 0·90 [0·89–0·90]) or in the west region (HR 0·91 [0·91–0·91]).
In the analyses limited to individuals who were vaccinated (table 3), all minority groups were 30–48% less likely than white people to have received the HDV, even after adjusting for age and gender (adjusted OR 0·59 [95% CI 0·59–0·60] for Black people; adjusted OR 0·58 [0·58–0·59] for Asian people; and adjusted OR 0·52 [0·52–0·53] for Hispanic people). Similar to overall SIV uptake, the gap narrowed to 26–32% after additonally accounting for region, income, chronic conditions, and patterns of health-care use (adjusted OR 0·68 [95% CI 0·68–0·69] for Black people; adjusted OR 0·71 [0·71–0·72] for Asian people; and adjusted OR 0·74 [0·73–0·74] for Hispanic people). This finding suggested that these factors might partly mediate, but not fully, the effect of race on HDV uptake. In the full model (which included terms for race and ethnicity), the strongest predictors of HDV uptake were receiving a low-income subsidy (adjusted OR 0·57 [95% CI 0·57–0·58] vs receiving no subsidy), residing in rural areas (adjusted OR 0·66 [0·66–0·67] vs residing in urban areas) or in the Midwest (adjusted OR 1·24 [1·24–1·25] vs the northeast), and having a chronic condition (adjusted OR 0·81 [0·81–0·81] vs not having a chronic condition). Frequency of hospital admissions and physician visits were not significantly associated with HDV uptake among individuals who were vaccinated.
The effect modification analysis (table 4; all ORs were estimated using white participants as the reference group) showed that for Black and Hispanic people, disparities in HDV vaccine uptake were more marked for those aged 65–74 years, women, urban dwellers, recipients of low-income subsidies, and for people who were more frequently admitted to hospital. Black women were 35% (adjusted OR 0·65 [95% CI 0·64–0·66]) less likely to receive an HDV than white women, whereas Black men were 30% (adjusted OR 0·70 [0·70–0·71]) less likely to receive an HDV than white men. Among Black people, more frequent physician visits were associated with a higher uptake of HDV and therefore a narrower gap compared with HDV uptake in white people. Among Asian people, urban residence was associated with lower uptake of HDV and therefore a wider gap compared with uptake in white people. For all minority groups, having an existing chronic condition was associated with higher HDV uptake and therefore a narrower HDV uptake gap compared with white people, whereas higher intensity of service use was linearly associated with a wider gap. Results from the effect modification analysis for receipt of SIV are shown in the appendix (p 1).
Discussion
We found that people from racial and ethnic minority groups were significantly less likely than white people to receive seasonal influenza vaccines during the 2015–16 season. This finding is not novel; in a 2019 meta-analysis,4 we found evidence of similar levels of disparities (30–40%) among Black and Hispanic people compared with white people, dating back to 2000.20 Our analysis, however, strengthens the evidence base because, unlike previous studies, we included the entire non-institutionalised US Medicare population (other than Medicare Advantage beneficiaries), and measured vaccine receipt using large population-based databases, thus avoiding sampling, social desirability, and non-response biases associated with surveys and self-reports of vaccine receipt.
This study also adds several novel and important findings arising from the rare opportunity afforded by the availability of two vaccines with the same indication and financial incentives, carrying similar recommendations from the Advisory Committee on Immunization Practices.1 First, we found racial and ethnic disparities in the uptake of a novel, more effective vaccine (HDV) even among people who received, and presumably wanted, influenza vaccination. These disparities, which were starker than disparities in SIV uptake, were observed in all minority groups, including Asian people, who had similar influenza vaccination rates to white people, which only further solidified within a few years after the introduction of the HDV vaccine. By limiting the analysis to people who were vaccinated, we were able to rule out several often-cited justifications for inequities in vaccine uptake, such as higher amounts of vaccine hesitancy and distrust of public institutions among minority groups, living circumstances (eg, homelessness), or limited physical access to preventive services.
Another important finding was that these disparities in uptake could not be fully explained by ethnic differences in age, gender, place of residence, Medicare status, pre-existing chronic diseases, intensity of health-care use, or region. Every person in our cohort had Part A and Part B Medicare coverage and, through modelling, we believe that we adequately accounted for racial and ethnic differences in sociodemographic and health-care use patterns, and for chronic diseases, which were associated with lower HDV uptake. The lower HDV uptake among people with chronic diseases was unexpected, as chronic disease is an indication for HDV use; further research is needed to confirm and explain this finding.
Taken together, these findings are alarming, because they point to a level of disparity in vaccine uptake that can hamper efforts to reduce the health and economic burdens of influenza, which remain substantial despite decades of intense public health efforts. From 2010–20, an estimated 9·3–45·0 million illnesses, 140 000–810 000 hospital admissions, and 12 000–61 000 deaths have been attributed to influenza, with adults aged 65 years or older representing the majority of those affected.24 Influenza burden is higher for Black people aged 65 years or older who tend to have higher rates of chronic conditions.25 Therefore, it is disheartening that this group has lower vaccination levels, even when compared with the already suboptimal levels among white older adults. Worse, we found that racial and ethnic disparities were compounded by gender, income, and regional disparities. Women, people on low incomes, and urban dwellers, who constituted a higher proportion of people of minority groups were less likely to receive a SIV. These findings are a worrying prediction for our ability to effectively use any future COVID-19 vaccines to control a pandemic that has disproportionately affected Black people and other minority groups.
Racial and ethnic inequities in health-care are pervasive and persistent; similar disparities have been observed for receipt of other vaccines, as well as other preventive measures, including cancer and hypertension screening.27 Our findings point to structural deficits systematically hampering access to influenza vaccination.4 Although it is possible that in some cases individuals from minority groups might have lower health literacy, greater difficulties in navigating the health-care system, or life circumstances that make it difficult to seek essential preventive services, these causes are themselves driven by deeply ingrained and often subtle systemic prejudices and discriminatory policies and practices.28 Internalised and interpersonal racism influencing interactions with health-care providers are other possible mechanisms.28 The effects of clinicians’ resources, working conditions, and of budgeting and resource allocation mechanisms at regional, state, and federal levels are also not well understood. New legislative, fiscal, educational, and research strategies are urgently needed to address vaccine uptake inequities.
Race and ethnicity are contested concepts, and attempts at measuring them are fraught with conceptual and practical difficulties.23, 29 To operationalise the concepts of race and ethnicity, we used the definitions and classifications used by the CMS and other federal agencies, despite their limitations. Undoubtedly, these categories do not capture the true extent of disadvantage in society, suggesting that gaps in vaccine uptake are likely to be wider for some subgroups; thus, our findings might understate the extent of racial and ethnic inequalities in vaccine uptake. Similarly, using a different approach to identify rural areas30 might reveal different patterns of inequality.
By relying solely on CMS data, it is almost certain that we underestimated the degree of vaccine uptake, as some vaccinations (eg, those administered during public health mass vaccination campaigns) might not have been captured in the CMS database. The extent to which SIV uptake is under-ascertained might vary between racial and ethnic groups, as it is possible that some groups are more likely to get vaccinated through public health mass vaccination campaigns and other programmes that are not included in the CMS database. However, there is no reason to suspect that the extent to which HDV uptake is under-ascertained in those captured in the CMS database varies by race and ethnicity.
Our findings might not be generalisable to influenza seasons in other years (for practical reasons, including data availability, we were unable to access data for more recent years). However, the pattern of inequities we described here has been remarkably constant since at least the late 1990s (eg, all four studies in a 2019 review showed 20–50% lower SIV uptake among Black people4) and, sadly, there is no reason to believe that the economic and social drivers of inequities have diminished in the past few years, as highlighted by poorer outcomes among minority groups during the COVID-19 pandemic.4, 31 To our knowledge, the 2015–16 SIV programme was not managed any differently from previous or subsequent programmes up to the present.
In our causal model, race and ethnicity was treated as an antecedent cause of most socioeconomic and medical determinants of vaccine uptake, such as income and chronic diseases, and therefore it cannot be confounded by these factors. However, our mediation analyses might have been biased by inaccurate measurement of these variables (eg, the variable low-income subsidy is an imperfect proxy for household income). We also did not have any information on other potential important mediators—eg, local availability of SDV and HDV, beneficiary immigration status, and English proficiency, as well as characteristics of their health-care providers such as providers’ knowledge and attitudes about vaccines, intentions to discuss available options, and behavioural tendencies. Research has shown that providers’ recommendations are influential in their client’s decision making process.32 Finally, our results might not be generalisable to all Medicare beneficiaries (eg, Medicare Advantage beneficiaries and those who do not have Part B and D coverage).
In the 2015–16 season, older adults from minority groups were less likely than white older adults to receive a SIV and, when vaccinated, were also less likely to receive the HDV. Inequities could not be fully explained by differences in sociodemographic factors, vaccine indications, and health-care use patterns. New legislative, fiscal, educational, and research strategies are urgently needed to address vaccine uptake inequities.
Contributors
SMM, ET, MML, AC, and GP were responsible for study design. AC and LLH were responsible for study supervision. LX was responsible for data analysis. LX and SMM accessed and verified the data. SMM drafted the manuscript. All authors reviewed and approved the manuscript. The corresponding author had full access to all of the data in the study and the final responsibility to submit for publication.
Declaration of interests
SMM has received unrestricted research grants from GlaxoSmithKline, Merck, Pfizer, Sanofi Pasteur, and Roche-Assurex for unrelated studies. SMM has received fees as a consultant and advisory board member for GlaxoSmithKline, Merck, Pfizer, Sanofi Pasteur, and Seqirus. ET, MML, and AC are employees of Sanofi Pasteur. LX, LLH, and GP report receiving grants from Sanofi Pasteur.
Data sharing
The authors are unable to share the data due to legal limitations of the data usage agreement with the CMS. However, the dataset used in this analysis is available from the CMS.
